
On the 30th anniversary of the Principles of Environmental Justice established at the First National People of Color Environmental Leadership Summit in 1991 (Principles of Environmental Justice), we continue to call for these principles to be more widely adopted. We propose an environmental justice framework for exposure science to be implemented by all researchers. This framework should be the standard and not an afterthought or trend dismissed by those who believe that science should not be politicized. Most notably, this framework should be centered on the community it seeks to serve. Researchers should meet with community members and stakeholders to learn more about the community, involve them in the research process, collectively determine the environmental exposure issues of highest concern for the community, and develop sustainable interventions and implementation strategies to address them. Incorporating community “funds of knowledge” will also inform the study design by incorporating the knowledge about the issue that community members have based on their lived experiences. Institutional and funding agency funds should also be directed to supporting community needs both during the “active” research phase and at the conclusion of the research, such as mechanisms for dissemination, capacity building, and engagement with policymakers. This multidirectional framework for exposure science will increase the sustainability of the research and its impact for long-term success.



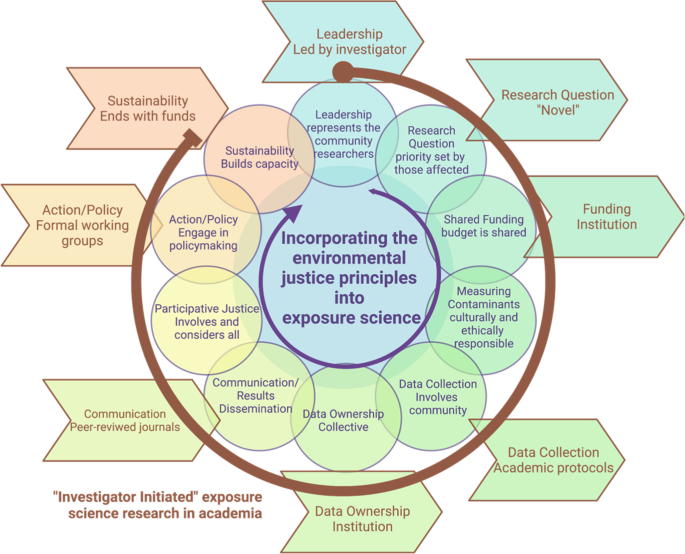
Exposure science is a multidisciplinary field that brings together researchers from various interdisciplinary areas that include risk assessment, epidemiology, public health, toxicology, environmental chemistry, public policy, and engineering [1]. At its core, exposure science seeks to answer basic questions such as: are people exposed to contaminant(s)? If people are exposed, what is the magnitude and intensity of the exposure(s) and what are the sources? Additional questions include: How are people exposed? What are critical routes and pathways of exposure? How can adverse exposures be mitigated? How can exposure mitigation strategies be sustainable? Answering these questions requires a detailed understanding of personal, cultural, behavioral, and political factors that contribute to these exposures, and how these vary by geographic regions, race, ethnicity, gender, socioeconomic status, and nationality [2]. Exposure science also seeks to better understand health risks associated with environmental exposures to inform exposure mitigation strategies suited for the affected population. While there is certainly value in this knowledge, we must dive deeper, as solely identifying exposures will not mitigate or prevent them. The view that science and data can speak for themselves has been widely accepted among scientists and perpetuated throughout the standard research process (Fig. 1). However, the traditional “investigator-initiated” academic approach rarely serves communities most affected nor leads to structural changes to improve public health. While the National Institutes of Environmental Health Science (NIEHS) translational research framework moves beyond the traditional “investigator-initiated” academic approach and highlights the importance of science informing practice and policy, it does not explicitly address structural racism as a root cause of health inequities [3]. Continuing to only characterize exposures without identifying root causes will not lead to meaningful changes, perpetuating distrust and failing affected communities. Herein, we bring a collective perspective to the exposure science field and advocate for community-driven approaches to not only identify harmful exposure(s), especially as they disproportionally affect marginalized communities, but to also reduce health disparities through community-centered approaches aimed at mitigating harmful exposures.
Over 30 years of research confirms that marginalized communities are disproportionately exposed to and affected by pollution [4, 5], hazardous waste sites [6], lead poisoning [7], hazards resulting from the built environment [8], food deserts [9], and other harmful environmental exposures [10]. In 2020 and 2021, these marginalized communities were repeatedly told that due to their economic status, ethnicity/race, occupations, and home location they faced a higher risk of morbidity and mortality due to COVID-19 [11,12,13,14]. These are the same communities in which researchers have documented elevated exposures to air pollution [15,16,17], increased rates of contaminated drinking water [5, 18], limited access to green spaces [19, 20], and disproportionate burdens from climate change [21]. While the field has often reported an association between these “risk factors” (e.g., higher levers of air pollution) and race/ethnicity, it has done so without considering the interpretation of these associations, ignoring that structural racism and not race is responsible for these differential exposures. The difference between a “risk factor” and structural racism is that structural racism encompasses the systems that reinforce and perpetuate racial discrimination [22,23,24]. For example, while housing, education, employment, and health care access individually can be referred to as “risk factors” the interplay between all of these is structural racism [24, 25]. This structure has led to disproportionate exposures and environmental injustices observed among marginalized communities. Marginalized communities continue to disproportionately face a mixture of harmful exposures [10], and socioeconomic inequality has grown [26], impacts from residential segregation persists [27], and many environmental exposure disparities have not been remedied [28,29,30].
Environmental justice (EJ) is defined as “the fair treatment and meaningful involvement of all people regardless of race, color, national origin, or income with respect to the development, implementation, and enforcement of laws, regulations and policies that affect the environment and/or public health” [31,32,33]. Since its inception, the EJ movement has been leading efforts to document environmental exposures and health conditions that reflect the values and needs of marginalized impacted communities [34]. The 17 Principles of Environmental Justice proposed at the First National People of Color Environmental Leadership Summit resonate just as strongly today as they did in the twentieth century (Table 1) [31]. The EJ movement calls for strict enforcement of informed consent, the right to a healthy environment, the need for involvement of all stakeholders in every step of the decision-making process, and public policy that is equitable. The Principles of Environmental Justice precede the 1994 federal Executive Order #12898 in the USA, which called for the integration of EJ in various branches of the government to serve “minority populations and low-income populations” [35]. Over the years, community-based EJ organizations have built power [36, 37], EJ scholarship has grown [38, 39], tools to assess and identify EJ communities have been developed [40,41,42], and research programs dedicated to combating environmental injustices have increased [43, 44]. Nonetheless, despite these arduous efforts, progress is still needed in translating these 17 principles into policies to support systemic change to reduce exposure disparities that result from historical and contemporary racist policies.
Advances in exposure science over the last 30 years have led to a need for guidance for the ethical reporting of exposure results to participants. This is particularly important when there is no clear outcome or interpretation of the results [93]. However, the relationship between measured exposure values and environmental health outcomes for many chemicals in use today remains unknown. Consequently, there are very few guidelines available today showcasing communication in personal exposure assessment research [94]. Historically, epidemiologists have claimed it is unethical to provide results to participants without clear established levels for interpretation, and that it would interfere and invalidate observational studies [93]. In this respect, exposure science is unique; levels associated with environmental health outcomes cannot be determined without first measuring the exposure. Exposure assessment thus often involves grappling with exposure values for which there is no clear interpretation [94]. However, this approach is evolving. Researchers report that participants have generally been able to manage anxiety arising from receiving results even when there are no clear health guidelines [95] and lessons for communication have been drawn from other fields [96]. The California Environmental Biomonitoring Program is required by statute to report all results to participants and as such has pioneered approaches for the release of results on complex chemical exposure to its participants [97]. Sometimes the results may be received after the research funding is ended. Again, as stated above, institutions or funding agencies could mandate funds for results report back to communities from EJ community-based research and for evaluation of those processes.
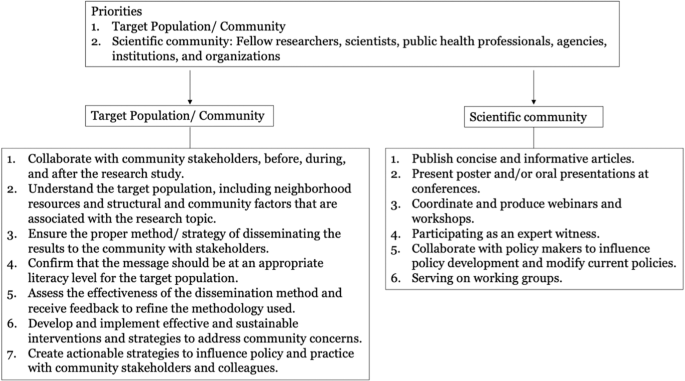
The EJ framework presented herein takes a multidirectional approach and proposes that the community should receive the research results before they are disseminated to the broader scientific community. Scientists able to interpret and present their findings and caveats in conference presentations and publications should also be able to present them to the community that provided them the samples. These presentations should include accessible explanations of the limitations and uncertainty of the study. Transparency should start prior to sample collection, so that the communities understand the limitations of the data to be collected and its interpretation. This transparency is particularly important in interpreting the exposures of underserved and understudied communities who may be most vulnerable. This may be achieved during the planning stages of the study in the community-engagement phase. While the peer-review process does add scientific validity to the findings, the long wait time between initial submission to publication means that participants may be placed in a state of uncertainty until individual or community dissemination occurs. Depending on the findings an appropriate timeline in coordination with community partners is an approach to determine when to best synthesize and report back study findings. The plan for data communication and dissemination should also be covered during the consenting process. While methodologies are still developing for the appropriate evaluation of the reporting back results, it is essential that we understand how communities are using this information to advance the environmental health and justice [98, 99].
Relying on communities as experts due to their lived experiences and how this expertise can be incorporated to advance partnerships is highlighted in the EJ principles (principle number 16). Through Ford and Airhihenbuwa’s (2010) Critical Race Framework, a similar concept is referred to as “Experimental Knowledge”, which overlaps with the educational term “Funds of knowledge” [51, 100]. This concept refers to “historically accumulated and culturally developed bodies of knowledge and skills essential for household or individual functioning and well-being” [61], in other words, due to their lived experiences community members possess invaluable knowledge that can be incorporated throughout the research design and dissemination strategy [61]. This practice will increase the effectiveness of the intervention while improving the scientific knowledge of the specific topic area within the community.
Equitable access to the benefits of exposure science raises concerns about participatory justice. This term refers to the direct participation of those most affected by a particular decision or policy. All communities involved should participate and benefit from exposure science activities in equitable ways. As an example, the state of California started community-led air pollution monitoring mandated by Assembly Bill 617 that seeks to address persistent air pollution hotspots in disadvantaged communities [101]. The California Air Resources Board (CARB) established a process through which communities can apply for enhanced monitoring and mitigation efforts CARB 2020. This avenue provides funding and increases attention to local EJ concerns, like those near the Port of Sacramento [102].
Although well intentioned, directing resources to communities could lead to skewed attention and funding toward communities with already well-established environmental and/or social justice organizations. For example, the list of applicants to the first round of the CARB Community Air Grant (in 2019) had many more applicants than could be awarded. Each application represented significant coordinated efforts and time for the applicants [102]. Communities with significant air exposures that lacked an experienced organization to prepare the application were missing from this list. In the proposed EJ framework, all communities would benefit from and participate in exposure science activities and achieve EJ, including those lacking the infrastructure, time, energy, and financial resources to coordinate such efforts. To make this possible, exposure scientists and funding agencies should actively support the participation of marginalized communities and direct resources such as paid internships or additional funding to the communities and assist them in applying for awards. In addition, barriers to ongoing community participation should be assessed and funds used to mitigate these barriers.
An EJ framework to exposure science engages a wide range of stakeholders and place the communities at the forefront. It is critical to consider the wide range stakeholders, inching policymakers, regulatory agencies, grassroots, and national non-profit organizations needed to move research toward actual change. Each of these stakeholders operates in a different sphere and tying these spheres together through an EJ framework is critical for reducing exposures. It is not enough for scientists to recommend individual reduction exposure behaviors; the field must evolve, identify, and demand structural changes. Training for exposure scientists must be interdisciplinary and address the importance of incorporating an understanding of the social and structural determinants of health for advocacy and action for effective public health change.
Traditional environmental health research that ends in a publication of no interest to the community or to policymakers charged with their protection is archaic. We are not calling for the end of publications, rather for community-driven science to not only develop scientific evidence but also to achieve engagement and action through an equitable, participative, and action-oriented process. Enacting local policies requires knowledge and access to yet a different set of players and rules, and most communities, scientists, and stakeholders are often unfamiliar, or unaware, of these critical individuals or groups. Some of this gap in knowledge is often filled by non-governmental organizations, who serve critical roles in building bridges with academic institutions and policymakers. While challenging, exposure scientists must incorporate an EJ framework to their work. This involves providing public comment on regulatory documents, serving on advisory boards, or actively engaging in workgroups. Ideally, these would be done alongside community members whose “funds of knowledge”, testimonials, and status as constituents have the collective power to enact real change [100, 103]. As these actions are often needed after the research funding has ended, to pay for efforts in this area, such as time for students/research assistants, institutions could voluntarily establish EJ-focused cost-sharing designed to release indirect resources, or there could also be cost-sharing mandates from the funding agencies as a condition of award acceptance. Federal grant funding agencies could also mandate that a certain percentage of the funds go toward investing time toward capacity building and translation/policy activities. Such funds could be used to support efforts either from the researcher/institution, by the NGO or community to disseminate findings to stakeholders and to prepare policy briefs and other actionable documents.
Sustainability of interventions and exposure mitigation strategies aimed at reducing the risk of harm and adverse health effects is paramount in marginalized communities suffering environmental health disparities. By sustainability, we mean implementing changes and knowledge gained via the research process that meets present needs without compromising the ability of future generations in the affected communities to meet and safeguard said changes. However, said sustainability is often dismissed, not incentivized, and not without its challenges to implement by both researchers and community stakeholders in the affected communities.
Current research practices often focus on initiating partnerships with affected communities to conduct the research. However, more often than not, these partnerships cease when all of the research data are collected, leaving communities alone to fight for action on the findings and never to hear from researchers again. Communities may be left with more questions than sustainable solutions to their environmental problems. Several factors may explain why said partnerships are not successful. First, building relationships and trust, establishing partnerships, and retaining those partnerships with impacted communities is labor and resource intensive. Establishing these partnerships can take months to years to build and requires that researchers effectively engage affected communities throughout the research process. Often, researchers are also not equipped with the appropriate staff and research team to engage with target communities, nor do they invest in providing the affected communities with resources to mitigate environmental health disparities. Still, it is important to highlight examples of successes in CBPR in exposure science. One such example includes initiatives conducted as part of the Center for the Health Assessment of Mothers and Children of Salinas (CHAMACOS) Study. CHAMACOS is the longest-running longitudinal birth cohort study of pesticides and other environmental exposures among children in a farmworker community in California. Programs such as the CHAMACOS Youth Council developed in collaboration with local community partners train local Latino youth in research design and implementation, promote environmental health literacy, and engage youth in advocacy and outreach [92]. As part of this program, trained youth have conducted field data collection that not only helps to promote careers in exposure science by exposing youth to the field, but also contributes to the success of ongoing studies, including those focusing on youth. In addition, the CHAMACOS study has successfully engaged members from underrepresented groups for training in environmental health sciences at all graduate and postgraduate levels helping to increase the pipeline in the field.
An EJ approach recognizes that community-engaged research is one key method for the suitability of partnerships [57]. Successful research teams not only recruit participants from EJ communities for their research studies, but also hire community members as part of their staff. A comprehensive team approach informs the research process and can support recruitment and data collection efforts. Moreover, it can help research teams understand the culture and practices of their target population, and the tools needed to be implemented to develop sustainable intervention strategies. Research in marginalized communities also needs to strive toward establishing and developing strategies to effectively build trust with these populations so that the burden does not fall entirely on new investigators who may not always have the necessary institutional support required to move forward during and after their research funding has ended.
A comprehensive EJ framework is necessary to ensure sustainability and requires implementation of a multi-pronged approach that includes co-leading, co-training, involves including junior investigators, ethnically and racially diverse research teams and leadership, capacity building, community mentors, and seeks to identify and implement evidence-based solutions that are sustainable.
Exposure science research has focused on the study of stressors and receptors in the context of space and time at the ecologic, community, and individual level. Nonetheless, hazard identification in the absence of social justice can exacerbate disparities in marginalized communities [104]. For example, following the quantification of harm associated with the chemical bisphenol A (BPA), exposure decreased among populations able to access alternative products, but BPA exposures were highest among low-income communities and those facing food insecurity [105, 106]. Another example is the identification of high levels of flame retardants in the bodies of residents of California, which led to the phasing out of some of these chemicals in new furniture, but continued exposure was documented for lower-income populations through their continued use of older or reused furniture [107, 108].
Exposure science needs to move beyond the individual and the mechanistic approach [109]. This is most evident in current exposome applications which are oriented toward personalized medicine [110]. As stated in Nwanaji-Enwerem et al. (2021), adopting a “compound” exposome approach would be an important step toward incorporating equity and EJ into exposure science [110]. That is to move from this individual approach, communities and human populations—and their exposures—should be seen as complex societies with economic relations, social classes, racism, sexism, cultural practices, and relationships to other species [2, 109]. This framework seeks to uplift the expertise and data from community organizations and the EJ movement, who are increasingly turning toward gathering their own data to understand their local environment and document environmental hazards [111]. Marginalization is not exclusive to race but it is often that exposures disproportionally affect communities of color [4]. Intersectionality offers a lens to analyze and incorporate attributes, such as LGBTQ identity, and disability, which are not discussed thoroughly in the EJ scholarship [112, 113]. Furthermore, peer-reviewed journals can help amplify this scholarship by calling for special issues and integrating researchers into their editorial boards whose methodology centers CRT, intersectionality, CBPR, and EJ.
Researchers should meet with community members and stakeholders to learn more about the community, involve them in the research process, collectively determine the environmental exposure issues of highest concern for the community, and develop sustainable interventions and implementation strategies to address them. Incorporating community “funds of knowledge” will also inform the study design by incorporating the knowledge about the issue that community members have based on their lived experiences [100, 103]. Institutional and funding agency funds should also be directed to supporting community needs both during the research and needs for dissemination, policy briefs, and other action at the conclusion of the research. This multidirectional framework for exposure science will increase the sustainability of the research and its impact for long-term success. In addition, involving the community in the research project, from start to finish, will facilitate community learning about exposure science and how it relates to the health of all those involved. It will also provide researchers with better knowledge of human behaviors, activities, and risk perceptions that may impact exposures, and improve researcher competency in assessing exposures. An EJ approach will increase a sense of belonging and improve communication among the community, the researchers, and other organizations involved [103].
Furthermore, it is not enough to document the continued exposure and environmental health disparities in structurally marginalized communities. We call for the incorporation of the EJ principles (Table 1) in exposure science to be the norm and not just words (Fig. 1). Along with critically engaging with this perspective, we hope to amplify the voices of those who are historically excluded in this work. As members of the research community from different sectors (e.g., academic, governmental, or non-profit institutions) and diverse backgrounds and lived experiences, we will seek to become better mentors, work toward institutional change that values and rewards EJ principles and speak up against injustices.
Marginalized communities are groups and communities that experience discrimination and exclusion (social, political, and economic) because of unequal power relationships across economic, political, social, and cultural dimensions.
We acknowledge that we reside on the stolen land of Indigenous People and we acknowledge the struggles of our ancestors who came before us. Moving forward we encourage that a portion of honorarium fees received for speaking on topics belonging to the community should be re-invested in programs that promote equitable health initiatives. The following scientists contributed to this framework: Sa Liu, Jon Levy, Pallavi Pant, Ryan G. Sinclair.
YOVH is supported by a Diversity Supplement through the National Institutes of Health under R01ES029598-03S1. CSA is supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under T32HD049311. LQA is supported in part by a NHLBI Career Development Award (K01HL138124). PIB is supported by the National Institutes of Health under P30ES006694. JEJ is supported by the National Institutes of Health under P30ES006694. MG is supported by NIH/NIEHS P50ES026102, NIH/NIEHS P42 ES025589, USEPA #83615701. The publication’s contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health, or the U.S. Environmental Protection Agency.